The uterus is normally held in place inside the pelvis with various muscles, tissues, and ligaments.
Because of pregnancy, childbirth or difficult labour and delivery, in some women, these muscles weaken. Also, as a woman ages, there is a natural loss of the hormone estrogen, that can lead to the uterus dropping into the vaginal canal, causing the condition known as a prolapsed uterus.
Some of the risk factors that can cause this condition are:
● Getting older, especially after menopause, when levels of circulating estrogen drop
● Pregnancy and childbirth
● Factors related to delivery, including trauma, delivering a large baby, or having a vaginal delivery
● Having a high body mass index (BMI)
● Frequent heavy lifting
● Straining during bowel movements (with constipation)
● Chronic coughing (with bronchitis and asthma)
● A history of pelvic surgery
● Genetic factors leading to weakened connective tissue
● Smoking
Symptoms include:
● Urinary leakage, retention or bladder infections
● Discomfort in the pelvic area
● Lower back pain
● Pelvic heaviness or pulling
● Vaginal bleeding or an increase in vaginal discharge
● Difficulties with sexual intercourse
● Uterine protrusion from the vaginal opening
In mild cases, there may be no symptoms. Symptoms that appear only sometimes often become worse toward the end of the day.
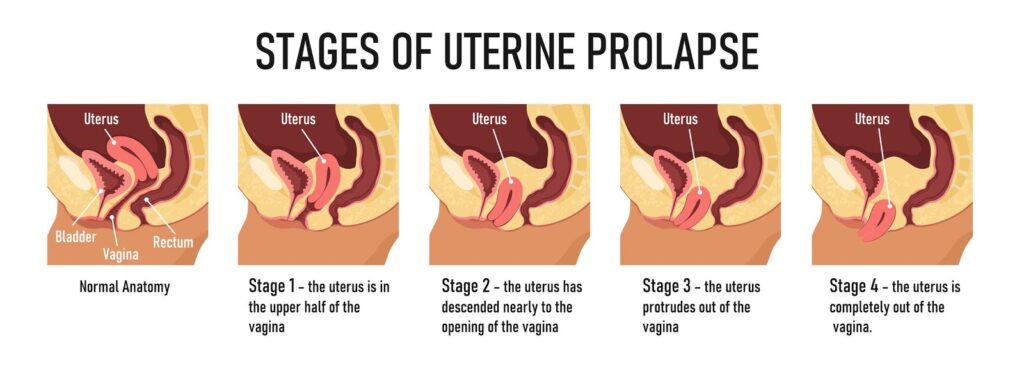
Stages
Uterine prolapse can be categorized as incomplete or complete:
● Incomplete uterine prolapse: The uterus is partially displaced into the vagina but does not protrude.
● Complete uterine prolapse: A portion of the uterus protrudes from the vaginal opening. The condition is graded by its severity, determined by how far the uterus has descended:
● 1st grade: descended to the upper vagina
● 2nd grade: descended to the introitus, which is the opening to the vagina
● 3rd grade: cervix has descended outside the introitus
● 4th grade: cervix and uterus have both descended outside the introitus
Diagnosis
A health care provider will ask about symptoms and perform a physical examination. While examining the pelvis, the provider will evaluate for organ placement and vaginal tone. An ultrasound or MRI may help assess the severity of the prolapse.
Treatment
Treatment depends on the stage and severity of the prolapse. Some strategies can reduce the risk of uterine prolapse developing and stop it from worsening. Prolapse up to the third degree may be helped with pelvic exercises and life style modifications..spontaneously resolve. More severe cases may require medical surgical treatment.
These include:
● Performing kegel exercises regularly and correctly, which help in strengthening the pelvic floor muscles
● Preventing and treating constipation
● Avoiding heavy lifting
● Using correct body posture whenever lifting is necessary
● Managing chronic coughing
● Maintaining a healthy weight through diet and exercise
● Considering estrogen replacement therapy during menopause
In cases where medical treatment is required for advanced conditions of uterus prolapse, the following options can be considered:
● Vaginal pessary: This is a vaginal device that supports the uterus and keeps it in position. It is important to follow the instructions on care, removal, and insertion of the pessary. In cases of severe prolapse, a pessary can cause irritation, ulceration, and sexual problems.
● Surgery: Surgical repair of a prolapsed uterus can be performed through the vagina or abdomen. It involves skin grafting or using donor tissue or other material to provide uterine suspension.
● A hysterectomy may also be recommended for advanced uterus prolapse conditions and where no future pregnancies are intended
Conclusion
If you have symptoms of uterus prolapse, visit a doctor or specialists for proper diagnosis and evaluation as well as to discuss treatment options. They can make recommendations for a treatment choice that will work the best for you.
Special Thanks to Dr Laxmi Shrikhande for the expert advice.